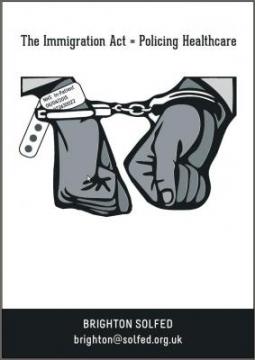
The Immigration Act = Policing Healthcare
Introduction
Healthcare should be available to all and not a few. The need for care outweighs any excuse to withhold or challenge someone’s access to healthcare, for example whether they have the ability to pay or where they have come from.
The Immigration Act of 2014 has far reaching strands that pushes society further to the right. It affects many areas of life such as housing and health. The aim of it is to punish those who are vulnerable and it is part of an ideology that is racist, which aims to divert attention away from those who benefit from capitalism, stigmatising other areas of society. They claim it is to finance a strained NHS, avoiding the real pressures being applied through marketisation and re-organisation.
This pamphlet, written by members of Brighton Solidarity Federation’s Health and Social Care Network, with support from Brighton Migrant Solidarity and Docs Not Cops, looks at how it is affecting the NHS and how it aims to make health workers do the dirty work of the government by policing the people they treat. This is through administrative oppression creating gatekeepers to health.
Only through organising and acts of solidarity can we repeal this act and put an end to it before it goes any further. We are all human and no one is illegal; the patient and worker will always come first.
This pamphlet is not definitive and is only guidance. As the political climate constantly changes, as do the laws they inflict on us. This pamphlet is based on the government’s information last updated on 25th March 2015. Check the Department of Health’s publications for updates:
https://www.gov.uk/government/organisations/department-of-health
Contents
+ Introduction
+ Immigration Act and Health
+ What this means for all healthcare staff
+ Discriminatory Practise
+ Economics
+ Who’s Next?
+ What can staff do?
+ Exemptions
+ Contacts
Immigration Act and Health
The government is increasing and introducing new charges for certain people for NHS hospital treatment. There are health care surcharges on visas for more than six months (£150 for students or £250 for others per year). Anyone who has not paid this surcharge and is not ordinarily resident in the UK may have to pay for inpatient services. There is a new pressure on medical staff to decide whether treatment is 'immediately necessary' or can be withheld. NHS trusts have to comply with these charges and recover the costs, which is now a legal requirement.
This affects non-EU-nationals who do not have a visa, and EU nationals without EHIC (European Health Insurance Card) or other health insurance. GP and A&E services remain free of charge, as charging only applies to inpatient services. There are some exemptions for a few vulnerable groups such as asylum seekers and refugees, and those who have been trafficked into the country.
The Secretary of State for Health can waiver any charges for a patient and their children and/or their companion travelling with them for ‘exceptional humanitarian reasons’. One motivation for these special cases will be what the political class feel they can exploit from these unfortunate situations. If they really cared, why not extend the exemptions to everyone?
To be classified as exempt from charges, evidence needs to be provided to the NHS body, who will then decide if it is successful or not and have to make “enquiries as it is satisfied are reasonable in all the circumstances”. The responsibility to provide evidence lies on the individual patient. What counts as suitable evidence for the Overseas Visitor Managers (OVMs) is guidance, and what is acceptable is down to the NHS body in light of the individual patient's circumstances.
Instituting this scheme will drive vulnerable migrants away from NHS services. It will force doctors and health services to question people’s immigration status, and to act like border guards. No one should be afraid to go to the doctor, either because they can’t pay or might be punished. People should not be racially profiled.
An important aspect that is highlighted by the government is that the success of these new laws will only be effective if all NHS staff (clinical, administrative and auxiliary) are aware and supportive of the OVMs. The only way we will be effective in supporting people and challenging racist discriminatory laws will be with our solidarity in not supporting OVMs and being aware of the damage the Immigration Act has on people and our society.
What this means for all healthcare staff
The key to implementation of the Immigration Act is both clinical and administrative staff engaging with the OVMs. Those coordinating implementation want all NHS staff to ‘raise the alarm’ to the OVMs when they suspect someone could be charged for services.
Clinicians have a further role in classifying treatment for patients, including:
-
To take the final decision as to whether treatment is immediately necessary, urgent or non-urgent.
-
To confirm that a patient is receiving treatment from exempt services.
-
To confirm that a patient is a victim of specified types of violence (torture, female genital mutilation, sexual or domestic violence). It is not expected that the clinician will be able to provide confirmation in all cases, in particular in respect of victims of torture, domestic or sexual violence where the cause of physical injuries and symptoms may not be immediately apparent.
-
to confirm the patient is fit to travel to return home for further treatment.
Immediately necessary treatment is that which is needed to save a patient’s life, or prevent a condition from becoming immediately life threatening, or to prevent permanent serious damage from occurring. For example, all maternity treatment is considered immediately necessary. NHS Bodies cannot refuse or withhold this treatment.
Urgent treatment is that which cannot wait to be treated in a patient’s ‘own country’ due to the potentially life threatening deterioration, pain or disability a particular condition is causing. NHS bodies again cannot refuse or withhold the treatment.
Non-urgent treatment is routine elective treatment that ‘could wait until the patient can return home.’ This treatment could be refused or withheld by NHS bodies.
By classifying the patient’s care as either immediately necessary or urgent does not make the treatment free, but means the NHS bodies cannot refuse the treatment. This means whether the patient is charged or not depends on other factors such as whether the OVM team knows of them, and whether the service or person is exempt from charging.
Patients can be charged retrospectively, even if they did not know they could be charged. However, the implementation document states that the relevant NHS body may write off debt due to a patient’s financial situation and thus 'it would not be cost effective to recover cost' or 'there are no further practical means of pursuing debt recovery'. The Secretary of State for Health may also waive any charges.
Remember, overall it is up to the OVM and NHS body to decide whether or not someone is exempt from charging. The patient will be asked to provide evidence but the OVM decides whether this is valid or not. In certain circumstances the clinician’s opinion will be sought to determine factors relating to a case.
Discriminatory Practise
Although claimed these new measures are not discriminatory, as they will apparently be checking everyone’s identity, they are. This is all about racial profiling and harassment. This is making the priority of health, someone’s immigration status. Clinical and administrative staff will not be expected to ask for evidence from patients, but will be expected to pass concerns onto the OVMs for ‘investigation’.
Universal healthcare only works if it is available to all. This creates a system of racism and discrimination, in conflict with equality policies at NHS Trusts. This Act will target vulnerable people who will not have the means to pay the charges. It will not benefit the NHS financially, as more time, money and effort is introduced into an increased bureaucracy. What’s more, the infrastructure is being put in place that could eventually be used to charge everyone.
Economics
One big issue for the implementation of the immigration act in the NHS was ‘Health Tourism’ which was a drain on the NHS. In 2012/13 this drain on resources was 0.1% of the NHS budget. The Department for Health’s own research reports “it’s impossible to estimate with confidence” the actual cost of deliberate use of the NHS as health tourism. If the implementation was based on economic grounds why are the real drains on the NHS such as PFI debts, costs of reorganisation, below average GDP spend on health not being tackled effectively?
The Health surcharge, which is an extra charge for visa applications, is an excuse to add further financial penalties to those wishing to come to the UK. People migrating here will already be contributing to ‘the system’ and health service. This is through living here by buying amenities, paying rent and paying taxes etc. Why is further charging being applied? Because they want to turn people away who will not be of benefit or able to provide some form of profit for the wealthy.
Part of the implementation is the introduction of profit and commercial charging into the NHS. Chargeable patients will be paying 150% of the tariff for treatment. This is the introduction of charges, where will it go next? Firstly its the people from outside Europe, secondly its the Europeans, then finally privatisation of healthcare full stop, where even if you are an ordinary resident of the UK you will have to pay.
Who’s Next?
The expansion of structures for charging patients is merely the latest iteration in a series of devices leading to marketisation of the NHS. Many have derived from initiatives of the Thatcher government (such as transitioning to outsourced cleaning staff), to others enthusiastically adopted under the most recent Labour government, such as the utilisation of Private Finance Initiatives in the funding of hospitals and lauding the internal market. This latest example is a particular concern though, as it threatens one of the foundational principles of the NHS, that of being free at point of need.
While charging immigrants may appear to be plausible on its face, in that they are not liable for the income taxes that contribute towards NHS funding, they are being charged as part of a calculated decision to isolate segments of the working class from each other. The idea is that as immigrants may be outside of our circle of sympathy, they’ll be easy to target in order to erode the principles of solidarity on which the NHS was founded. The transition to other vulnerable sections will be much more convenient for the ruling class once the principle of fee recovery has been established.
It is already possible to gather which groups will be targeted by looking at contemporary arguments against the implementation of public healthcare in the US. For instance, Jerry Brown, the Governor of California, managed to deflect a nascent movement towards public health by claiming that he did not want to spend tax dollars on treating the ailments of smokers. Similar arguments have been used in regards to obesity, with proposals to charge obese individuals for their treatment. These methods of framing the debate completely alter our approach to health, by coercing us to view health from the perspective of an individual consumer. In reality, the social context inhabited by an individual will contribute greatly to whether they take up smoking or are capable of abstaining once starting and obesity follows both a class gradient and an egalitarian gradient in industrialised societies, in that those with the least resources in the least equal industrial societies are far more vulnerable to it.
To return to the conception of health as a social benefit, we must also consider that the very principle of insurance accedes to the notion of collective responsibility and shared risk. It is also worth considering one of the claimed detractions from public healthcare in the claim that it’ll be unsustainable given the projected demographic shift of the next decade. The rejoinder to this is fairly obvious in that we can address such issues far more rationally by acting in concert than in imbuing the market with our faith.
There are fairly well chronicled inspections districts in the UK during their initial industrialisation attesting to what occurs when there are no provisions for those no longer capable of providing wage labour.
What can staff do?
We believe you need to be aware of the OVMs, but that we should not be supportive of what they stand for, their role and their work. The patient should be at the heart with any decision. Before any action relating directly to the patient, they must have knowledge of what is happening and the potential outcome of any action or non-action will have. Knowing there are people willing to support in differing ways will be reassuring and a start to collectively undermining this act. Do not forget that patients can be charged retrospectively so understanding the consequences of actions has a real impact on patients.
How to make the work of OVMs difficult is dependent on many factors such as the will of staff, patients, consequences of actions, the area of work and the support available.
Some potential ideas could be:
-
Put in Freedom of Information requests for information on whose identities are being checked i.e. racial profiling
-
Support patients in pressuring OVMs to accept exemptions
-
Boycott of OVM services
-
Non-communication with OVMs
-
Communication Blockades
-
Wrong information being provided (Sabotage)
-
Demonstrate outside offices
-
Delay, boycott, avoid bureaucratic processes such as relevant paperwork
-
Set up clinics to avoid the Home Office
-
Do not ask migration details from patients
-
Do not send out migration letters
Contact Brighton Solfed’s Health & Social Care Network to help organise in your workplace. The collective will be much more effective than the individual. If you are not in Brighton there will be many groups able to help or point you in a direction.
Get in contact as we want to organise in your workplace, inform and support patients and challenge this racist ideology.
Brighton Solfed is part of the Anarcho-Syndicalist Union Solidarity Federation, which is affiliated with the International federation of labour unions, the IWA. The Health & Social Care Network is a campaign initiated by Brighton Solfed with the aim of organising within this sector. We believe by acting together workers can directly tackle issues and assert our and patients rights. We’re holding meetings promoting mutual support and solidarity, where issues can be shared and collectively acted on.
Brighton Solfed’s contact details can be found in the contacts section towards the end.
Exemptions
Non-Chargeable Patients
-
Anyone who is an ‘Ordinary Resident’ of the UK.
-
Whether a person is ordinarily resident in the UK is essentially a three-fold test (four-fold for non-EEA nationals) assessing whether that individual:
-
is lawfully in the UK;
-
is here voluntarily – it will be rare for a person not to be in the UK voluntarily;
-
and is properly settled here for the time being;
-
and in the case of non-EEA nationals subject to immigration control, has ILR (Indefinite Leave to Remain) in the UK.
-
Anyone from the European Economic Area member state or Switzerland with a valid European Health Insurance Card or Provisional Replacement Certificate or for elective treatment has a S2 document.
-
Any non-European Economic Area national who has paid the Health Surcharge
-
Prisoners and Immigration detainees
-
Anyone in whose case the Secretary of State for Health determines there to be exceptional humanitarian reasons to provide a free course of treatment. This exemption will also apply to their child and/or companion who is authorised to travel with them, for whom the exemption is limited to treatment that cannot await their return home.
-
Refugees, (those granted asylum, humanitarian protection or temporary protection by the UK).
-
Asylum seekers, (those applying for asylum, humanitarian protection or temporary protection whose claims, including appeals, have not yet been determined).
-
Individuals receiving support under section 95 of the Immigration and Asylum Act 1999 (the 1999 Act) from the Home Office.
-
Failed asylum seekers receiving support under section 4(2) of the 1999 Act from the Home Office or those receiving support under section 21 of the National Assistance Act 1948 from a Local Authority.
-
Children who are looked after by a Local Authority.
-
Victims, and suspected victims, of human trafficking, as determined by the UK Human Trafficking Centre or the Home Office, plus their spouse/civil partner and any children under 18 provided they are lawfully present in the UK.
Non-Chargeable Health Services
-
accident and emergency (A&E) services, this includes all A&E services provided at an NHS hospital, e.g. those provided at a walk-in centre or urgent healthcare centre. This does not include those emergency services provided after the overseas visitor has been accepted as an inpatient, or at a follow-up outpatient appointment, for which charges must be levied unless the overseas visitor is exempt from charge in their own right;
-
services provided outside an NHS hospital, unless the staff providing the services are employed by, or working under the direction of, an NHS hospital;
-
family planning services (does not include termination of pregnancy);
-
diagnosis and treatment of sexually transmitted infections;
-
treatment required for a physical or mental condition caused by:
-
torture; female genital mutilation; domestic violence; or sexual violence,
-
except where the overseas visitor has travelled to the UK for the purpose of seeking that treatment.
When identifying a survivor of torture, FGM, domestic or sexual violence (and other cruel, inhuman or degrading treatment or punishment) to establish if an exemption applies, an OVM should accept:
• confirmation from a medical professional, including a referring GP, who could most appropriately identify signs and symptoms of torture and that the treatment accessed is attributable to this torture; and/or
• confirmation from an appropriate non-governmental organisation or charity, such as the Helen Bamber Foundation or Freedom from Torture Foundation, confirming that the patient is a client of theirs and is accessing their services as a survivor of torture.
Exemptions of diagnosis and treatment of specified infectious diseases:
-
acute encephalitis
-
acute poliomyelitis
-
anthrax
-
botulism
-
brucellosis
-
cholera
-
diphtheria
-
enteric fever (typhoid and paratyphoid fever)
-
food poisoning
-
haemolytic uraemic syndrome (HUS)
-
human immunodeficiency virus (HIV)
-
infectious bloody diarrhoea
-
invasive group A streptococcal disease and scarlet fever
-
invasive meningococcal disease (meningococcal meningitis, meningococcal septicaemia and other forms of invasive disease)
-
Legionnaires’ Disease
-
leprosy
-
leptospirosis
-
malaria
-
measles
-
mumps
-
pandemic influenza (defined as the ‘Pandemic Phase’), or influenza that might become pandemic (defined as the ‘Alert Phase’) in the World Health Organization’s Pandemic Influenza Risk Management Interim Guidance
-
plague
-
rabies
-
rubella
-
severe acute respiratory syndrome (SARS)
-
smallpox
-
tetanus
-
tuberculosis
-
typhus
-
viral haemorrhagic fever (which includes Ebola)
-
viral hepatitis
-
whooping cough
-
yellow fever
Contacts:
Brighton Solfed / Health & Social Care Network
- Organising in your workplace and community
07790607310
Links:
This list is by no means exhaustive but includes links that have been brought to our attention.
Solidarity Federation
- Anarcho-Syndicalist Union
International Workers Association
- International of Anarcho-Syndicalist Unions
Brighton Migrant Solidarity
- Campaigning for migrants locally
www.brightonmigrantsolidarity.noblogs.org
Doctors of the World
- Health Advocacy and Clinics
Docs Not Cops
- Campaign group around Immigration Act
Medical Justice
- Rights for detainees
Hackney Migrant Centre
- Free Advice for Asylum Seekers,
Refugees and Recent Migrants
www.hackneymigrantcentre.org.uk
Praxis Community Projects
- Wide variety of Advise for Migrants
The AIRE Centre
- EU Migrant Advice
Refugee Council
- Directory of Services Available and Advise
Migrant English Project
- Free Informal English Lessons in Brighton
Joint Council for the Welfare of Immigrants
- Advice and Resources on Immigration
www.jcwi.org.uk Call: 02075537470
Asylum Aid
- Legal Advice for Asylum Seekers
www.asylumaid.org.uk Call: 02073549264
| Attachment | Size |
|---|---|
| 356.93 KB |